
Acidosis and hyperkalemia may also lead to capture failure. (Figure.2) Causes of failure to capture include lead dislodgment and elevated thresholds due to fibrosis or exit block at the site of lead implantation. It is characterized by a pacing spike on the surface electrocardiogram at programmed heart rate, which is not followed by an evoked potential (P or a QRS). įailure to capture is defined as the inability of pacing impulse to produce an evoked potential.
#Failure to capture pacer spikes generator
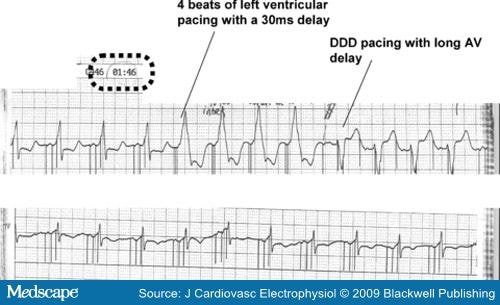
(Figure.1) Causes of output failure include lead fracture, generator failure, and inhibition of pacing due to over-sensing and crosstalk. It is characterized by the absence of a pacing spike on an electrocardiogram, and device interrogation confirms the diagnosis. It is defined as the inability of the pacemaker to generate an impulse resulting in a heart rate lower than the programmed lower rate limit. This review will discuss the common pacing system problems of a cardiac implantable electronic device (pacemaker). The periodic evaluation of an implanted pacemaker is necessary to optimize programming and to identify correctable problems. ĭespite their success, electronic pacemakers have limitations, including complications related to implantation, limited battery life, the potential for infection, lack of physiologic autonomic responsiveness, and size restriction in younger patients. This process leads to excitation-contraction coupling resulting in the contraction of myocardial tissue. These pacing devices provide an external electrical stimulus that leads to depolarization of myocytes and helps maintain the electrical excitability of the heart tissue. The current standard of care for symptomatic bradyarrhythmias due to conduction system diseases is the implantation of a cardiac implantable electronic device. Acquired conditions such as myocardial infarction, age-related degeneration, procedural complications, and drug toxicity are the major causes of the native conduction system malfunction. Several diseases and conditions affect the conduction system by involving impulse generation, impulse propagation, or both. The failure of this intrinsic electrical conduction in the heart can result in different arrhythmic problems. This movement of electric potential in an orderly manner controls the rhythmic contraction of the heart's chambers. This innate electrical potential moves from the sinoatrial node to the atrioventricular node and finally into the His-Purkinje system. The cells present in the sinus node have innate automaticity, which starts the electrical activity in the heart. The sinoatrial node acts as the natural pacemaker of the heart. This functioning of the heart depends on the cardiac conduction system, which includes impulse generators (e.g., sino-atrial node) and the impulse propagating (His-Purkinje) system. The human heart is a pivotal organ in the circulatory system, and it beats more than 2 billion times during normal life.


 0 kommentar(er)
0 kommentar(er)
